The delicate balance catching stray tumor cells
Vulvar cancer can arise from chronic inflammation or from infection with high-risk human papillomaviruses (HPV). Vulvar cancer often spreads first to nearby lymph nodes and once it spreads it is hard to treat. Lymph nodes are our body’s filtration system and immune cells accumulate here to detect, contain and kill stray pathogens or cancers. The lymph nodes ‘downstream’ of a tumor are particularly crucial and often the first site where a metastatic tumor develops.
Within the lymph nodes, immune cells known as T cells perform several specialized roles in deactivating cancers. However, T cells are powerful killing machines that must be kept in check to prevent the destruction of healthy cells. As such, T cells have several regulatory checkpoints to maintain the balance between killing hostile and healthy cells. It is these checkpoints and regulatory controls that cancers exploit to swing the balance in their favor. Understanding how primary tumors manipulate the immune landscape of neighboring lymph nodes could provide better treatment and control of vulvar cancer.
Discovering the weakness in the immune balancing act
The research team isolated cells from surgically removed lymph nodes that were responsible for directly draining lymph fluid and migrating cells from a vulvar tumor. They then performed immune cell profiling and functional analyses on these lymph nodes, some of which already contained tumors. This allowed them to chart possible pathways used by tumor cells to weaken the immune response. They found two key changes in lymph nodes that appeared to be related to possible spread of tumor cells:
- More regulatory T cells which suppress immune responses;
- Fewer helper T cells (ICOS+ effector helper T cells) which direct other immune cells to act as cancer cell assassins.
Our findings reveal that different immune suppressive mechanisms may facilitate the initial spread of the primary tumor to the lymph nodes and subsequent metastatic growth,”
says Tanja de Gruijl, a professor of Translational Tumor Immunology from the Department of Medical Oncology and head of the Immunotherapy Lab at Cancer Center Amsterdam.
Rebalancing the scales
Decreasing regulatory T cell frequencies and enhancing the potency of the depleted helper T cells may be a viable strategy to rebalance the immune response. One way to do this is by reducing the checkpoint controls placed on the helper T cells. This would increase their potential to activate effector immune cells in the fight on cancer. The checkpoint in question is a cell surface receptor called CTLA-4. Blocking the CTLA-4 receptor may increase the impact of helper T cells, while keeping regulatory T cell numbers in check and thus prevent metastasis of vulvar tumors to the lymph nodes. “Our results point to future treatment options that could effectively curtail metastatic spread of vulvar cancer to and through the lymph nodes, and so considerably improve the outlook for patients,” says Prof. de Gruijl.
Read the full article here.
For more information contact: Professor Tanja D. de Gruijl (td.degruijl@amsterdamumc.nl).
Text by Lynita Howie.
People involved affiliated with Amsterdam UMC: Marijne Heeren and Jossie Rotman (PhD students), Gemma Kenter (gynaecologist), Maaike Bleeker (pathologist), and Katja Jordanova and Tanja de Gruijl (immunologists), departments of Obstetrics and Gynecology, Pathology, and Medical Oncology. Collaboration with Henry Zijlmans (Gynecologist), Netherlands Cancer Institute. Gemma Kenter and Henry Zijlmans are affiliated with the Center of Gynecological Oncology Amsterdam.
Funding: This work was supported by a research grant from the Dutch Cancer Society (KWF) and by the Louise Vehmeijer Foundation.
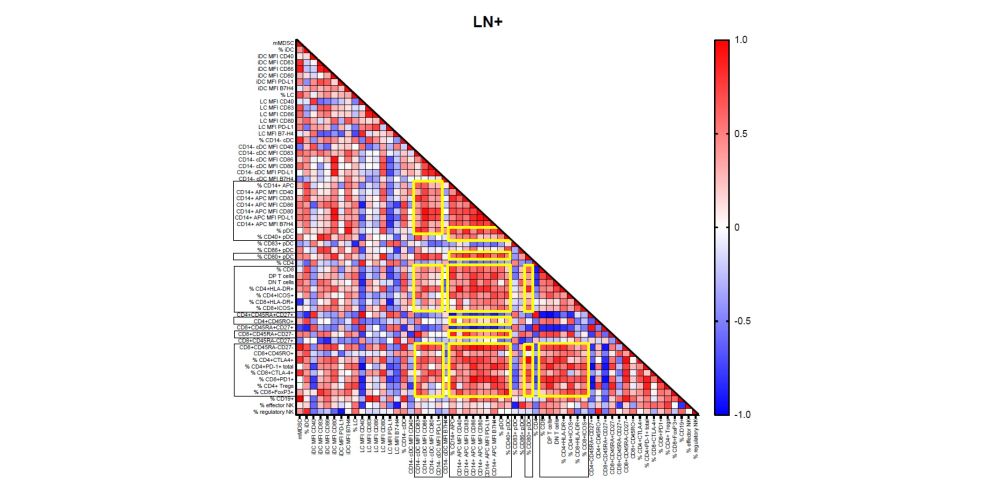 The figure shows a correlation matrix, demonstrating coordinated regulation of various immune suppressive immune subsets in lymph nodes invaded by vulvar tumor cells.
The figure shows a correlation matrix, demonstrating coordinated regulation of various immune suppressive immune subsets in lymph nodes invaded by vulvar tumor cells.

