Immunotherapy is a type of cancer treatment that stimulates a person’s own immune system to fight cancer. The ability of the immune system to recognize cancer cells as “foreign invaders” is tricky, as tumor cells arise from normal cells within our own bodies and are sometimes not identified as being different. In addition, as a tumor grows it often evolves and finds ways to hide from the immune system.
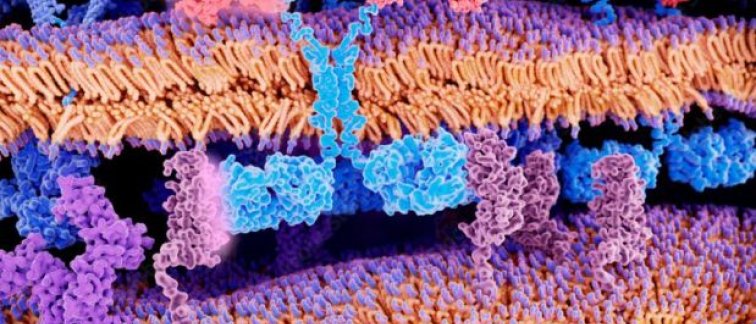
With Chimeric antigen receptor (CAR) T-cell therapy, a patient's own immune cells are modified in a laboratory – where they are given the ability to ‘see’ the malignant cells – and returned to the patient to eliminate their cancer. CAR T-cell therapy has proven to be effective for a number of cancers originating from the blood, bone marrow or lymph nodes.
For some patients, CAR T-cell therapy can save their lives
CAR T-cell therapy is currently used to treat a limited number of blood-related cancers, and patients only qualify if they are sufficiently fit to withstand the serious side effects common with this treatment. This immunotherapy is achieving long-term survival for approximately 40% of patients who had run out of other treatment options. Amsterdam UMC has now treated around 50 patients with lymph node cancer, and more than half are still in remission after more than two years. This is a remarkable medical achievement, taking into account their limited life expectancy of a median of 6 months before the availability of CAR T-cell therapy.
Providing clear information and improving the quality of life
Marie José Kersten, Professor of Hematology, has lobbied at the national level for the introduction and implementation of CAR T-cell therapy in the Netherlands, including getting this treatment reimbursed. She also coordinates Amsterdam UMC’s involvement in several large national and international research consortiums. In 2020, Prof. Kersten obtained multiple research grants to implement CAR T-cell therapy faster for more patients, and investigate the impact of this immunotherapy on patients’ well-being and quality of life. Prof. Kersten explains: "CAR T-cell therapy does not work for everyone: only forty percent of treated patients have long-lasting benefits. We want to develop materials that support the patient during the entire process. It is precisely the voice of the patient and informal caregiver we listen to: what is needed to better guide them during that 'voyage'?” The goal is to determine the best way to educate patients, their support team, and treating physicians so that everyone knows what they can expect before, during and after the treatment.
Can in-house CAR T-cell therapy save time and money?
A consortium of academic hospitals in the Netherlands, headed by Tom van Meerten from UMC Groningen, and including Amsterdam UMC, Radboud UMC and Erasmus MC, received a 30-million-euro subsidy from Zorginstituut Netherlands and ZonMw in 2020. The academic centers plan to compare in-house CAR T-cell production with commercial sources to see if savings in time and costs can be achieved. Prof. Marie José Kersten is also involved in this project. “A quicker throughput time is very important to these patients. It’s precisely this group who needs the treatment fast because they don’t usually have other options and have rapidly progressive disease, which is sometimes prohibitive for CAR T-cell therapy due to the waiting time during manufacturing,” says Prof. Kersten.
Faster and cheaper CAR T-cell production would also significantly improve accessibility for more patients. Currently, treatment per patient costs around € 350,000 for the cells and the consortium aims to reduce that to € 80-100,000. CAR T-cell therapy is so expensive because the entire treatment must be developed from start to finish for each patient individually. It also takes about four to six weeks before the lab-engineered immune cells can be given to the patient using an international commercial partner. Some patients simply do not have that time. The consortium aims to reduce production time to two weeks, as well as possibly improving the quality of the CAR T-cells by avoiding the freeze-thaw processes necessary for shipping.
Increasing therapy accessibility through research
CAR T-cell therapy is also being explored for other cancer types. Amsterdam UMC Professors of Hematology Tuna Mutis, Sonja Zweegman, and Niels van de Donk, along with Dr. Maria Themeli, are investigating the use of CAR T-cells for the treatment of multiple myeloma, in which cancerous plasma cells hinder the creation of healthy blood cells in the bone marrow and induce bone destruction. "We started treatment of multiple myeloma patients without other available treatment options with CAR T-cell therapy with exceptionally good results. These patients are seeing a substantial gain in survival benefit,” says Prof. van de Donk. In addition to applying the immunotherapy to this disease, Prof. Mutis and Dr. Themeli are working on standardizing the process of CAR T-cell creation so that it becomes available for a broader group of patients.
CAR T-cell therapy will become cheaper over time, like everything in medicine. What we strive for is a ready-made off-the-shelf CAR-T medicine directly available for patients. Prof. Tuna Mutis.
“Off-the-Shelf” CAR T-cell therapy
Dr. Maria Themeli and colleagues at the department of Hematology recently won an award for their abstract 'Generation of Universal “Off-the-Shelf” CAR-T from Induced Pluripotent Stem Cells' at the European CAR T-cell meeting. Rather than producing CAR T-cells from a patient’s own cells, which are sometimes compromised by the cancer, her team is investigating creating CAR T-cells from a type of stem cell. “The existence of a readily-available CAR-T product would greatly benefit the broader use and success of CAR T-cell therapy,” says Dr. Themeli. “There are still hurdles to be overcome, but I am convinced that in the near future, CAR T-cells derived from universal stem cells will have a place in the treatment of hematologic and other malignancies.”
Commitment to the future
Despite astounding success against some tumor types, immunotherapy does not yet work for everyone or every type of cancer. New discoveries are needed to better understand how tumors suppress the immune system, and to identify predictive biomarkers and explore new combination therapies. Towards achieving this, Cancer Center Amsterdam Foundation has financially committed to the establishment of Amsterdam ImmunoTherapy Center. With this investment, Cancer Center Amsterdam aims to become an internationally leading immunotherapy center committed to providing the best possible care for cancer patients.
For more information, contact cca@amsterdamumc.nl
[Credits] Text by Laura Roy. Parts of this article were adapted from “Je eigen afweercellen als medicijn” by Mieke Zijlmans in JANUS with permission. Amsterdam UMC - Janus