The human immune system defends our bodies against external attack from pathogens as well as internal attack from cancerous cells. Malignant cells are equipped with an arsenal of weaponry to evade immune attack. One such weapon is immune suppression, and it is used successfully by head and neck cancer tumors. These cancers, more specially known as head and neck squamous cell carcinomas (HNSCC), create a tumor microenvironment that reduces the toxicity of natural killer cells. Natural killer cells are roving cells that can invade tumors and, as the name suggests, kill cancer cells as a first-line defense.
Multiple lines of defense
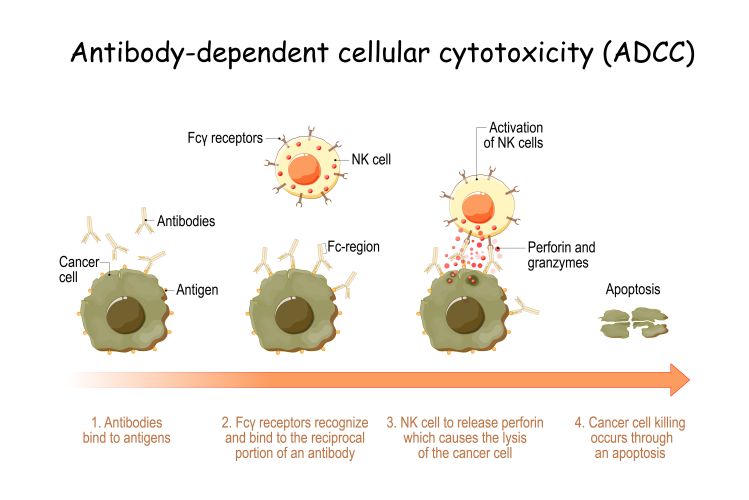
In response to cancer growth, our immune system employs a second, more targeted, line of defense by making antibodies. Antibodies are specialized proteins that bind to cancer cells and can restrict their uncontrolled growth. In the treatment of cancer, we can add a third line of defense by introducing artificial antibodies that enhance the natural antibody response. This is known as antibody therapy and, for HNSCC, the artificially produced antibody is called cetuximab.
A strategy with limited success
Cetuximab was approved for use 15 years ago as a much anticipated weapon against HNSCC. The antibody suppresses tumor growth by both neutralizing a growth signal receptor on the surface of cancer cells and triggering the immune system to attack the targeted cell.
However, the results of the treatment were disappointing. Although cetuximab bound to cancer cells successfully, the overall impact on tumor size was minor: treatment outcome improved only temporarily or for a minority of patients. “The immunosuppressive character of head and neck cancers may explain the relatively low response rates to this antibody immunotherapy,” suggests Mandy Gruijs, lead author and PhD student at Cancer Center Amsterdam.
Success with a two-pronged attack
The research team suspected that cetuximab may be more effective if natural killer cells were given a boost to counteract immunosuppression. This ‘boost’ came in the form of a molecule called ligand Pam3CSK4 that binds to a receptor on natural killer cells. Specifically, the Pam3CSK4 ligand binds to the Toll-like Receptor 2 on natural killer cells, amplifying the message that a pathogen is present. In a laboratory setting, the combination of cetuximab and ligand Pam3CSK4 enabled natural killer cells to infiltrate deeper into tumors, be more toxic to cancer cells, and release more pro-inflammatory cytokines and chemokines. “The combined therapy resulted in a significant delay in tumor growth or even complete tumor regression, and improved overall survival in preclinical models,” says Mandy Gruijs.
A promising tactic
The successful attack on HNSCC tumors using the combined therapy promises to improve the clinical outcomes of cancer patients. Gruijs predicts that, in the future “this treatment could well be applied together with other therapeutic strategies such as anti-PD-(L)1 checkpoint inhibition to further overcome immunosuppression by tumors.”
Read the article in The International Journal of Molecular Sciences.
For more information, contact the corresponding authors: Rieneke van de Ven, or Jantine Bakema.
This research was funded by Cancer Center Amsterdam and the Fjoer Foundation.
Researchers from Cancer Center Amsterdam: Mandy Gruijs, Sonja H. Ganzevles, Marijke Stigter-van Walsum, Richard van der Mast, Cornelis W. Tuk, C. René Leemans, Ruud H. Brakenhoff, Marjolein van Egmond, Rieneke van de Ven and Jantine E. Bakema.
Text by Lynita Howie
Photos: Adobe Stock