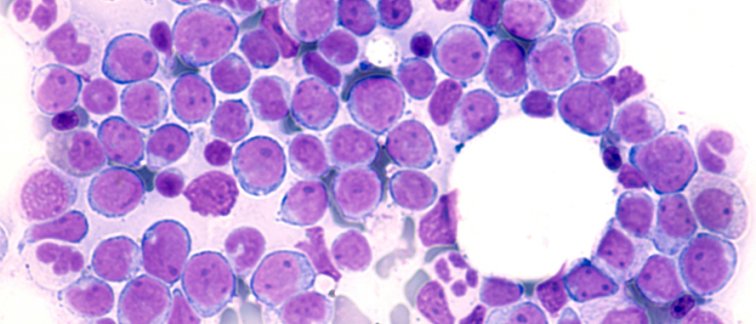
Acute myeloid leukemia (AML) is a relatively rare type of cancer with nearly 800 new patients diagnosed in the Netherlands annually. AML is characterized by an overproduction of immature leukemic blast cells in the bone marrow. These leukemic cells take over the bone marrow compartment, resulting in a general lack of normal blood cells (anemia), bleeding, risk of infection, and fatigue. AML patients typically receive chemotherapy with the aim to achieve a complete remission, potentially followed by a bone marrow stem cell transplantation to prevent disease relapse.
Prognostic Value of Measurable Residual Disease in AML
To see how an AML patient is responding to treatment, several diagnostic techniques have been developed to detect ‘measurable residual disease’ (MRD). These tests inform further clinical decision making as the presence of residual disease correlates with an increased risk of relapse. Nevertheless, 34% of AML patient with a negative MRD test result are still confronted with a relapse of the disease. Publishing in the journal Leukemia, a research team at Cancer Center Amsterdam led by Jeroen Janssen and Jacqueline Cloos aimed to refine MRD diagnostics by identifying underlying causes for false negative outcomes.
Does Hemodilution Hamper Accurate MRD Diagnostics?
To determine MRD status, a bone marrow (BM) sample serves as the source material for diagnostic tests that detect the presence of leukemic blast cells. However, these BM biopsies can be affected by blood ‘contamination’, as the BM is highly vascularized. In addition, dilution of the BM sample by peripheral blood is more likely to occur as more BM is aspirated.
Prof. Jacqueline Cloos explains, “Hemodilution - the presence of peripheral blood cells in bone marrow samples – decreases the leukemic burden and therefore ability of the test to detect measurable residual disease in AML patients. So, we searched for a diagnostic marker that can flag hemodiluted samples, marking them as a potential cause of a false negative test result.”
Mast Cells and Granulocytes as Diagnostic Markers of Hemodilution
The research team focused on the recognition of cells in patient biopsies that are exclusive for the bone marrow or peripheral blood. “We looked for the presence of bone marrow-specific mast cells and blood-associated granulocytes in patient samples to establish a formula that could detect hemodilution,” says first author Jesse Tettero. “We noticed that the first bone marrow aspiration usually provides a more reliable sample for MRD assessment than consecutive samples - which are more likely to contain peripheral blood cells.”
For more information contact Jacqueline Cloos, or read the publication:
Tettero, J.M., Heidinga, M.E., Mocking, T.R. et al. (2024) Impact of hemodilution on flow cytometry based measurable residual disease assessment in acute myeloid leukemia. Leukemia. https://doi.org/10.1038/s41375-024-02158-1
Researchers affiliated with Cancer Center Amsterdam
Jesse M. Tettero,
Maaike E. Heidinga,
Tim R. Mocking,
Glenn Fransen,
Angèle Kelder,
Willemijn J. Scholten,
Alexander N. Snel,
Lok Lam Ngai,
Costa Bachas,
Arjan A. van de Loosdrecht,
Gert J. Ossenkoppele,
David C. de Leeuw,
Jacqueline Cloos
Jeroen J. W. M. Janssen (currently at Radboud University Medical Center)
Text by Henri van de Vrugt.
This article was created for Cancer Center Amsterdam.
Follow Cancer Center Amsterdam on LinkedIn & Twitter /X.
© 2024 New Haven Biosciences Consulting– All rights reserved.