In the Netherlands, Canada and Australia routine population screening for cancer, including colorectal cancer (CRC) screening, has been disrupted due to the ongoing COVID-19 pandemic. This increases the risk of more CRC cases being detected at a later stage, leading to worse health outcomes and a likely increase in avoidable CRC-related deaths.
“Given the unpredictability of the coronavirus, it can be expected that the healthcare system will remain strained. We used mathematical modelling to investigate what would be the best strategy for resolving the backlog and preventing as many late diagnoses and unnecessary deaths as possible, without increasing the pressure on healthcare resources," says Francine van Wifferen, PhD candidate at the Department of Epidemiology and Data Science at Amsterdam UMC, and co-first author on the study published in Journal of Medical Screening.
Colonoscopy prioritization
During the first wave of the pandemic, the colorectal cancer screening program in the Netherlands and Canada was discontinued for two months. Six months after the disruption, screening services were still not operating at full capacity in Canada, while in the Netherlands full capacity was reached one month after the disruption. In Australia, the screening program was not completely suspended, and operated at 50% capacity for two months. Therefore, the researchers assumed that, on average, screening was disrupted for three months. Using this three-month disruption as a starting point, the researchers modeled a number of different scenarios. Two main variables were investigated: extending the recovery period in which missed individuals are caught up, meaning a longer screening interval for a larger proportion of the population, and increasing the detection threshold that flags a screening test positive.
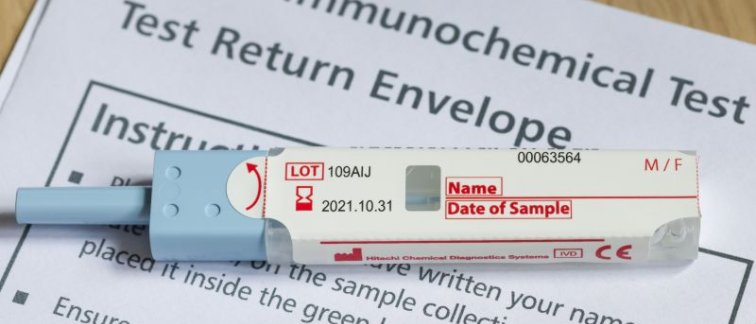
The screening test that is used in the Dutch screening program is the fecal immunochemical test (FIT). This test detects blood in the stool, with the amount correlating to the risk of colorectal cancer. Raising the detection threshold that defines a positive result means less people would be referred for colonoscopy, a visual examination of the colon to check for abnormalities. In an already strained healthcare system, this strategy aims to direct resources to individuals with the highest risk.
Model predictions
Van Wifferen: “For the Netherlands, the model predicted that if referral services can operate at 50% higher levels than pre-pandemic capacity during a six-month recovery period, we can almost completely eliminate the negative effect of a three-month disruption to screening while using the regular FIT threshold. Extending the recovery period to 12 or 24 months would greatly reduce demand for additional colonoscopies and still avoid most excess CRC-related deaths.”
If the healthcare system remains under pressure and screening capacity is limited, the researchers concluded that modestly increasing the FIT threshold during a 24-month screening recovery period would still prevent 30%-60% of excess CRC-related deaths. However, “catching up with the backlog using an extended recovery period prevents more excess CRC-related deaths than resolving the backlog by means of an increase in the FIT threshold. Thus, longer recovery periods should be considered while limiting the increase in the FIT threshold.”
The models predicted that large increases in the FIT threshold for an extended recovery period would increase excess CRC-related deaths rather than prevent them.
Real-world implications
The authors note that “the real-world impact of the COVID-19 pandemic on excess CRC-related deaths may be larger than predicted in this study because longer disruption periods have been observed than our simulated 3-month disruption, and some screening programs did not restart immediately at full capacity after the disruption.”
Van Wifferen concludes: “Although our models are based on the first COVID-19 wave, the results can still be used to guide decision-makers in how to manage colonoscopy resources to limit the excess CRC-related deaths, especially as the COVID-19 crisis persists, with new variants emerging and vaccines not being equally available globally.”
The study was part of the COVID-19 and Cancer Global Modelling Consortium (CCGMC; www.ccgmc.org), which was established to support decision making in cancer control both during and after the COVID-19 crisis.
Read the research article here:
Francine van Wifferen*, Lucie de Jonge*, et al. (2021) Prioritisation of colonoscopy services in colorectal cancer screening programmes to minimise impact of COVID-19 pandemic on predicted cancer burden: A comparative modelling study. Journal of Medical Screening.
*These authors contributed equally to this article.
For more information contact: f.vanwifferen@amsterdamumc.nl
Involved researchers at Cancer Center Amsterdam:
Francine van Wifferen, PhD student at Decision Modeling Center Amsterdam UMC, location Boelelaan.
Marjolein J.E. Greuter, Assistant Professor, Epidemiology and Data Science.
Veerle M.H. Coupé, Associate Professor, health-economic modeling in cancer.
Funding: The Dutch National Institute for Public Health and Environment, Cancer Council New South Wales and Health Canada
Text by Laura Roy