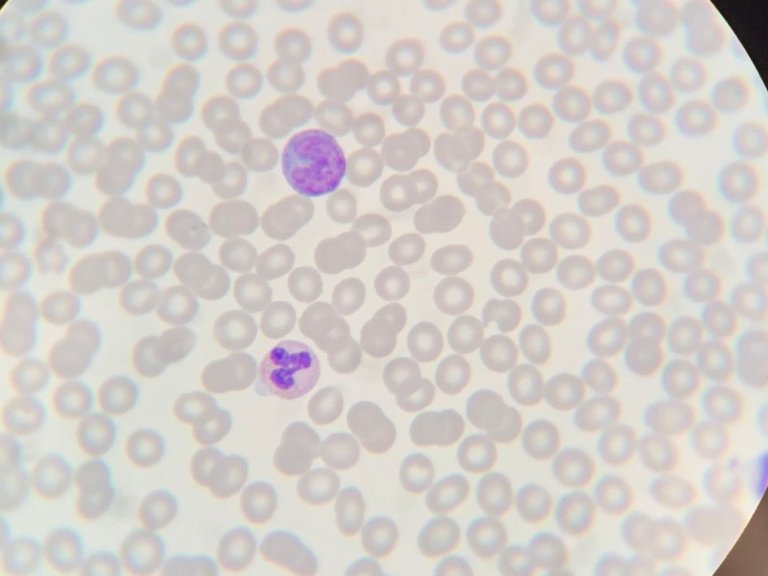
Prabath Nanayakkara, professor of internal medicine at Amsterdam UMC, has been working on increasing efficiency in acute care for years and recently, blood cultures have been the focus of his attention. Primarily, because the often don't provide the information that doctors and nurses are looking for.
"We're used to doing it this way but that doesn't mean the analysis is necessary. Certainly 'not when you look at the numbers. Of all the blood cultures that are done in the emergency room, only 15% indicate that something is wrong. It's even more interesting if you take a closer look at those positive results. Then about half of the positive blood cultures turn out to be false positives," says Nanayakkara.
AI can change healthcare
In Dutch A&Es alone, hundreds of blood cultures are taken every day, and the aforementioned figures gave Nanayakkara and his team the reason to look for a way of doing things differently. Nanayakkara: "We shouldn't do things in healthcare that aren't necessary. In addition, this is pre-eminently an issue in which AI can be used. In doing so, we are showing that AI can really change healthcare," he says.
"If this study is successful, we will not only reduce the number of blood cultures – and therefore the costs - but also ensure that the number of false positive blood tests decreases and thus, no patients will be treated unnecessarily. False positive results lead to uncertainty among patients and doctors, extra procedures, excessive treatment with antibiotics and, longer hospital admissions and even higher mortality in that group," he adds.
Clinical trial
Of course, reducing the number of blood cultures must be done safely so that infections are not missed. Amsterdam UMC will now start a clinical trial, the ABC study, to test the algorithm previously developed by the acute AI team in practice. This algorithm has already been extensively tested and validated nationally and internationally.
The trial is one of the first randomized controlled trials worldwide to use a similar algorithm in acute care. "Based on vital data from the electronic health record, such as body temperature and other standard lab results that provide information about possible infections, the algorithm can identify patients with a low risk of infection or inflammation. With this prediction, the doctor, together with his or her own observation, can better consider whether a blood culture is really necessary.
This prediction is now built into the electronic patient record (EPD) at Amsterdam UMC. When requesting a blood culture in the intervention group, the healthcare provider is shown this prediction on the computer screen, which is unique. With tailor-made advice for each patient, we expect to drastically reduce unnecessary cultures, hopefully by up to 30%," concludes Nanayakkara.