Annually, over 500,000 children die from diarrhoea, a preventable tragedy. Despite the efficacy of the straightforward ORS (Oral Rehydration Salts) powder – a blend of salts and sugars – its infrequent prescription raises questions about the persistent gap between knowledge and action. In this article Vanessa Harris, Assistant Professor of Global Health at Amsterdam UMC, shares her vision.
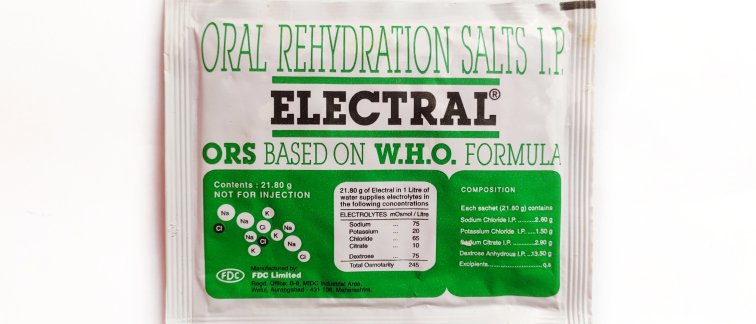
ORS (Oral Rehydration Salts) powder, when dissolved in water and consumed in small quantities during severe diarrhoea, prevents dehydration by facilitating rapid fluid absorption into the bloodstream and better retention in the intestines.
ORS is cost-effective, proven, and globally available. Scientists are perplexed by its underuse during childhood diarrhoea cases, considering most doctors are aware of its benefits, exposing a common "know-do gap."
Diarrhoea, the third leading cause of death among children in low- and middle-income countries, underscores the urgency for effective solutions. Dr. Vanessa Harris, Assistant Professor of Global Health at Amsterdam UMC, emphasizes that inadequate sanitation often contributes to this alarming statistic.
While the causes of diarrhoea vary, the rotavirus, causing watery diarrhoea, is a major concern, and underuse of ORS is a significant issue in such cases. Despite the existence of a rotavirus vaccine, its effectiveness varies across countries. Other factors, including bacterial and parasitic infections leading to a bloody variant, may necessitate antibiotics.
What drives poor quality of care for child diarrhoea?
A quarter of global child diarrhoea deaths occur in India. A joint study by researchers from American and Indian universities investigated the ORS dilemma in private clinics in Bihar and Karnataka states. As many as 2282 doctors were visited for the study, in 253 villages. The researchers hypothesized three potential explanations before the investigation: unavailability, low cost (leading doctors to prefer more profitable options), or the perception of ORS as not a 'real medicine' due to its simplicity as a powder. To test these hypotheses, actors posed as fathers seeking help for a two-year-old with diarrhoea at private clinics, explicitly asking for ORS or antibiotics. Even with sufficient ORS stock in some clinics, results were striking.
The study, published in Science, revealed that although 86% of surveyed doctors claimed they would prescribe ORS, only 28% did so when not explicitly requested. Instead, 69% provided unhelpful antibiotic prescriptions. Financial incentives or stock availability played minor roles, remaining consistent whether actors obtained the medication themselves or if there was limited stock.
Interestingly, when patients specifically asked for ORS, 55% received it—nearly doubling the prescription rate. The primary issue, as summarized by researcher Neeraj Sood, was that "doctors believe patients do not want ORS." The physician's perception of patient desires played the most significant role, with the belief that a simple powder does not meet patient expectations.
The authors stress the study's importance, suggesting that lives can be saved by educating patients about the significance of ORS and addressing implicit assumptions with doctors. Real patient surveys indicate no aversion to ORS.
Dr. Harris praises the study as a "creative and significant exploration of a pervasive problem." She suggests similar mechanisms may operate in other countries, making India not necessarily an exception. Dr. Harris notes a study limitation, suggesting actors should have included a sick child, as physicians might be more inclined to prescribe ORS when faced with clinical signs of dehydration. Harris also recommends supporting parents with sick children rather than urging them to be more assertive. Ensuring everyone has ORS at home through local health services could be an option.
Drought and flooding
Considering climate change's potential contribution to global outbreaks, the Amsterdam UMC leads a consortium investigating diarrhoea diseases and climate change, the SPRINGS consortium. Floods and heavy rains can contaminate water sources, while droughts may increase the prevalence of the rotavirus due to longer water storage periods.
The consortium will focus on specific regions in Tanzania, Ghana, Italy, and Romania. Identifying vulnerable areas and proposing interventions will help prevent diarrhoea diseases, considering factors like contaminated food due to flooded agricultural areas or inadequate sanitation. Dr. Harris hopes to incorporate new ORS insights into these studies, emphasizing the crucial role of this remedy.
Source: this article is a revised version of an article originally published in Dutch in Trouw, authored by Elleke Bal. Access the original piece here.
Learn more about Dr. Harris by reading our previously published articles:
Tackling the effect of climate change on diarrheal diseases (February 2024)
Grants for GLORIA progamme (February 2022)
Using rotavirus vaccines to fight antimicrobial resistance (January 2022)
Follow Amsterdam institute for Infection and Immunity on LinkedIn & Twitter/X.