Alzheimer’s disease biomarkers
Alzheimer’s disease (AD) on MRI is characterized by hippocampal and temporoparietal atrophy and are commonly used as MRI biomarkers. However, this MRI biomarker does not reflect disease state as well as the underlying pathophysiological mechanisms. Pathologically, AD is characterized by amyloid-beta plaques and phosphorylated-tau (p-tau) neurofibrillary tangles (NFT) in the grey matter. Previous studies, using MRI and PET imaging, already showed tau tracers on PET images correlate with cortical atrophic patterns on MRI, while amyloid-beta deposition does not. However, PET imaging has limited resolutions, therefore this study investigated the association between post-mortem in-situ MRI cortical thickness and histopathological hallmarks in pathologically-confirmed AD subjects.
MRI and pathological biomarkers
In the study, 19 AD and 10 non-neurological control brain donors underwent post-mortem MRI scans. Upon subsequent autopsy, regions were immunostained for amyloid-beta, p-tau and reactive microglia. Next to this, post-mortem MRI was also compared to antemortem MRI of the same AD donors. Their findings showed that in AD, amyloid-beta load correlates with a slightly increased cortical thickness relatively to the atrophic AD cortex. P-tau is the strongest contributor to regional cortical atrophy in formal and temporal regions. Finally, reactive microglia load is the strongest correlate of cortical atrophy in the parietal regions. Distinct histopathological markers correlate thus differently with cortical atrophy.
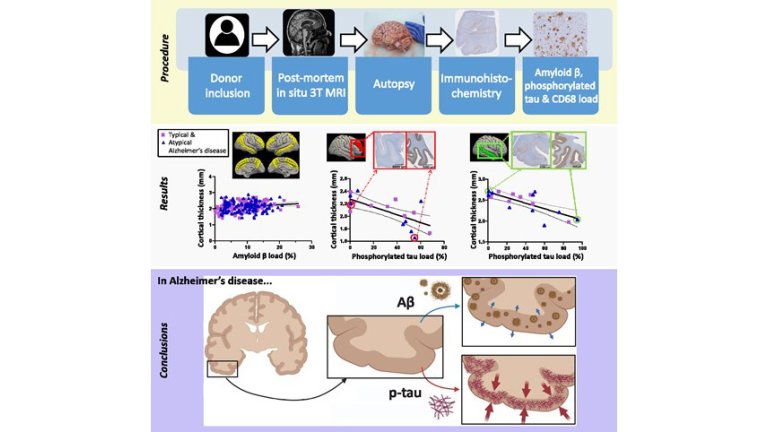
Next to this, they also explored within the AD phenotypes, and showed that reactive microglia load is increased in atypical AD, but not in typical even though no differences were found in MRI-pathology associations. Moreover, the study also showed that post-mortem in situ MRI can be used as a proxy for ante-mortem in-vivo MRI.
Read the publication in Brain Communications: Amyloid-β, p-tau and reactive microglia are pathological correlates of MRI cortical atrophy in Alzheimer’s disease

