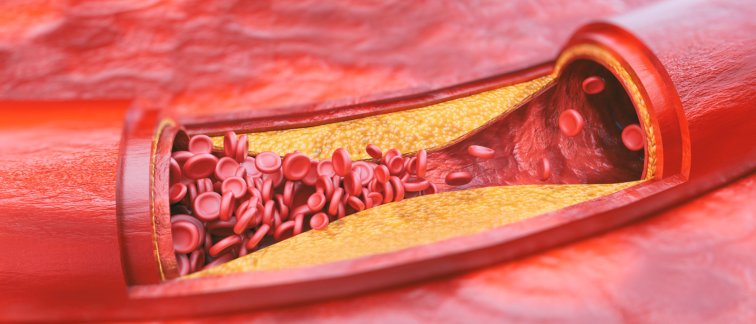
The underlying cause of the majority of cardiovascular diseases is atherosclerosis. Due to the formation of atherosclerotic plaques, life-threatening atherothrombotic events, including myocardial infarction or stroke, may arise when these plaques rupture or suffer from erosion.
Recent clinical trials in patients have revealed that lowering inflammation is an important strategy for combating cardiovascular disease. However, these anti-inflammatory immunotherapies were not developed specifically for cardiovascular disease and therefore exhibited suboptimal efficacy and induced unwanted side effects.
Immune checkpoint proteins to propagate or halt immune-cell activation in atherosclerosis
The team of Esther Lutgens has discovered that co-stimulatory immune checkpoints play a central role in the pathogenesis of atherosclerosis. Her team has developed novel small molecule-based therapies based on inhibiting immune checkpoint signaling intermediates, in this case the interaction between the immune checkpoint CD40 and the signaling intermediate TRAF6.
In experimental proof of concept studies, her team has shown that these are efficient and safe immune-therapeutics for the treatment of atherosclerosis.
Current projects in the lab
Identifying the immune checkpoint landscape in atherosclerosis
We are currently answering the question of which cell types express which immune checkpoints in which stage of atherosclerosis. The lab uses single cell technologies such as mass-cytometry and single cell RNA-sequencing to generate the immune checkpoint atlas of cardiovascular disease.
Unraveling the role of recently identified immune checkpoint proteins in atherosclerosis
The family of immune checkpoints is expanding. We are currently identifying the immunogenic properties of these novel members, as well as their effects on atherosclerosis.
From bench to bedside: bringing our CD40-TRAF6 small molecule inhibitor to the clinic
Our proof of concept studies on blocking CD40-TRAF6 interactions in atherosclerosis showed a spectacular decrease in atherosclerosis without inducing immune suppressive side effects. We are currently optimizing the chemical and pharmacokinetic properties to be added to the translational pipeline.

Use of animal models in atherosclerosis research
Atherosclerosis is a complex, multifactorial disease which cannot be mimicked using a ‘lab on a chip’ approach. As the interactions between many different immune cell types, flow, shear stress, hyperlipidemia and endocrine factors all affect its pathogenesis, we make use of living organisms, especially mice.
However, in the Lutgens’ lab, we aim to reduce the number of laboratory animals that we use by carefully designing our experiments, and by testing aspects of the disease (i.e. production of inflammatory mediators, or cell migration) as much as possible in in vitro systems. Moreover, we use a virtual ligand screening and computer-based modeling approach to design the best small molecule inhibitors possible.
We are convinced that more and more ‘lab on a chip’ methods will be developed, thereby reducing the numbers of laboratory animals needed. However, as atherosclerosis is a complex, multifactorial disease, it is likely that we will always have to rely on laboratory animals to properly study this disease and design treatments for humans.